Alzheimer's disease is a devastating neurodegenerative disorder that affects millions of people worldwide. Improved techniques for detection and intervention could change the trajectory of the disease for countless sufferers and their families and carers.
Newly published research in Science Translational Medicine by researchers from Washington University has opened up the possibility of using the gut microbiome as a risk assessment tool to determine the likelihood we may go on to develop Alzheimer’s disease.
The study involved a large cohort of participants, both with and without Alzheimer's, whose gut microbiome was analysed using advanced sequencing techniques. The findings revealed significant differences in the gut microbiota composition between the two groups, suggesting a potential link between the gut and the changes that occur in the brain that eventually lead to the neurodegeneration seen in Alzheimer’s disease.
Alzheimer’s Gut-Brain Connection
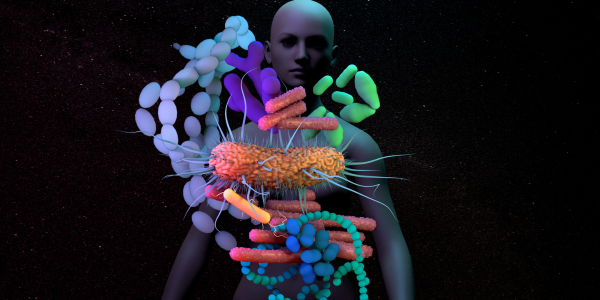
It is well established that we have a bidirectional communication pathway between the gut and the brain, known as the gut-brain axis. We know that our gut microbiota play a vital role in regulating this axis by producing various metabolites and neurotransmitters that can influence brain function, mood and behaviour.
Whilst it’s already well-documented that Alzheimer’s disease patients exhibit altered microbiome populations, what hasn’t been well-explored in previous research is how early these changes begin, and if they can be used to track risk. By studying the gut microbiome, researchers aim to understand how alterations in microbial populations may contribute to Alzheimer's disease development. By gaining this understanding, we may be able to identify opportunities to implement specific gut-mediated support that might slow or mitigate these risks.
Promising Insights
This new study identified specific microbes that were associated with increased or decreased Alzheimer's risk. Certain beneficial bacteria, such as Bifidobacterium and Lactobacillus, were found to be more prevalent in individuals with a lower risk of developing the disease.
Conversely, harmful microbes like Bilophila and Escherichia were more abundant in those at higher risk. These findings open up new avenues for potential interventions, such as probiotics or targeted antimicrobial strategies, to modulate the gut microbiota and reduce Alzheimer's risk.
If further research can confirm these newer findings, the use of the gut microbiome as a pre-clinical assessment tool for Alzheimer's risk could revolutionise early detection and prevention strategies. This would open the door for preventative care using non-invasive techniques to analyse an individual's gut microbiome composition. It will give healthcare professionals opportunities to identify those at higher risk of developing Alzheimer's, potentially years before symptoms manifest.
Healthy Gut, Healthy Mind, Healthy Body.
Whilst further research is needed to confirm the precise microbiome signatures needed to detect Alzheimer’s disease risk, this research further emphasises the importance of optimising gut function and supporting digestion when it comes to brain wellbeing. As scientists continue to identify the mysteries of the gut-brain connection, we inch closer to a future where Alzheimer's disease can be intercepted before it takes hold, changing countless lives for the better.
REFERENCES
Ferreiro AL, et al. Gut microbiome composition may be an indicator of preclinical Alzheimer’s disease. Science Translational Medicine 2023 Jun 14;15(700)